Getting a pedicure with nail fungus requires proper precautions. Clients should inform salon staff beforehand, allowing for preparation with hospital-grade disinfectants and sterilized tools. Bringing personal, pre-sterilized implements offers added protection, while specialized medical pedicures provide safer alternatives with dry techniques and antifungal products. Individuals should postpone appointments if experiencing active infections, open wounds, or compromised circulation. Proper communication and choosing reputable establishments with documented sterilization protocols greatly reduce transmission risks during treatment.
Key Takeaways
- Inform the salon about your nail fungus in advance so they can prepare with proper disinfection protocols and specialized tools.
- Choose salons offering medical pedicures with Certified Master Pedicurists who use hospital-grade disinfectants and sterile equipment.
- Opt for dry pedicures to minimize water exposure that can worsen fungal conditions and reduce transmission risk.
- Bring your own pre-sterilized tools if allowed by the salon to eliminate cross-contamination concerns.
- Continue antifungal treatments before and after pedicures, scheduling sessions every 4-6 weeks for continuous care.
Understanding Nail Fungus: Symptoms and Causes
Toenail fungus presents a common yet troubling condition for millions of individuals seeking routine foot care, affecting approximately 10% of people worldwide with its characteristic symptoms of nail thickening, brittleness, and discoloration. This condition, medically known as onychomycosis, typically begins at the nail edge, causing yellowing, whitening, or browning of the affected nail, which may eventually crumble or detach from the nail bed entirely.
The primary culprits behind these fungal infections are dermatophyte fungi, particularly Trichophyton rubrum, which thrive in warm, moist environments like sweaty footwear. Individuals with compromised immune systems, especially those with diabetes, face a 30% higher risk of developing toenail fungus. Additionally, athletes frequently exposed to damp conditions and older adults with reduced circulation experience higher incidence rates, with nearly 50% of people over 70 affected.
The Risks of Getting a Pedicure With Fungal Infections

Why would anyone risk transforming a relaxing pedicure experience into a potential health hazard? Nail fungus creates serious complications when introduced to salon environments, particularly through improperly sterilized tools that facilitate the spread of infections to other clients and staff members. Contaminated footbaths serve as ideal breeding grounds for pathogens, increasing the risk of infection even when technicians follow standard protocols.
The consequences extend beyond the salon, as inadequate disinfection practices using non-hospital-grade solutions can create a domino effect of transmission throughout the establishment. Individuals with compromised immune systems, especially diabetic patients, face heightened dangers of developing secondary bacterial infections that may progress to systemic health complications. Additionally, EPA research confirms that exposing fungal infections to salon environments can introduce microorganisms through microscopic skin breaks, potentially worsening existing conditions. Ensuring proper disinfection, including effective disinfectant solutions, is essential to prevent these risks.
Communicating With Your Salon: Transparency Matters
When seeking professional nail services with a fungal infection, transparency becomes the cornerstone of responsible salon interaction. Individuals should inform salon staff about toenail fungus prior to their appointment, allowing professionals to implement their established protocols for handling contagious conditions. This advance notification enables the salon to prepare appropriately with hospital-grade disinfectants, sterilized tools, and disposable items specifically designated for the service. Reputable salons typically maintain specific guidelines for addressing fungal infections, including isolation of tools and specialized disinfection procedures that comply with health standards. By disclosing the presence of infection, clients actively participate in preventing cross-contamination between customers and staff. This ethical approach guarantees the salon can maintain their hygiene standards while accommodating the client’s needs, ultimately fostering a safer environment for everyone involved in the service process. Ensuring proper disinfection practices is essential to avoid spreading the fungus to other clients or staff members.
Essential Sterilization Practices to Look For

Selecting a salon with rigorous sterilization protocols represents the cornerstone of safe pedicure services for clients with nail fungus. When evaluating a salon’s proper sterilization practices, clients should verify that all tools undergo autoclaving, a high-pressure steam process at 121°C that eliminates 99.9999% of microorganisms, preventing cross-contamination effectively. Reputable establishments clean and disinfect surfaces with hospital-grade, EPA-approved solutions, maintaining the recommended 10-minute contact time for maximum efficacy against fungal spores. Clients should inquire about the salon’s use of disposable implements, such as nail files and buffers, which eliminate transmission risk entirely for those specific items. Additionally, thorough establishments maintain daily sterilization logs documenting their disinfection procedures, demonstrating compliance with state health regulations and offering transparency regarding their commitment to sanitation standards. Implementing antibacterial cleaning wipes for nails can further enhance hygiene practices by ensuring tools and surfaces remain thoroughly sanitized between clients.
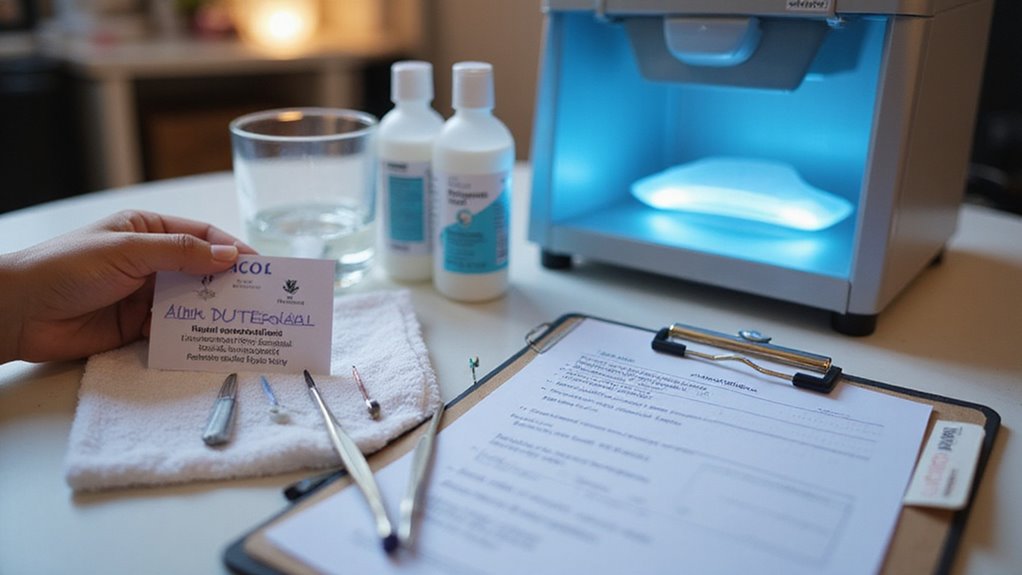
Bringing Your Own Tools: A Safer Alternative

For individuals managing nail fungus, bringing personalized, pre-sterilized pedicure tools represents one of the most effective strategies to minimize cross-contamination risks during salon visits. Clients can thoroughly disinfect their tools using ethyl alcohol, submerging implements for at least 10 minutes to eliminate fungi and bacteria on all surfaces.
Alternatively, running personal tools through a dishwasher at temperatures exceeding 140°F provides thorough sterilization, effectively neutralizing potential pathogens. Proper maintenance of a personal pedicure kit requires consistent cleaning after each use, preventing fungal buildup and ensuring safety for subsequent appointments.
Before scheduling an appointment, clients should contact the salon to confirm their policy regarding customer-provided tools, ensuring staff will accommodate and properly handle these sterilized implements during the service, creating a safer pedicure experience for those with nail fungus.
Specialized Salons That Handle Fungal Conditions

Specialized medical pedicure salons offer a much safer alternative for individuals with nail fungus, providing thorough treatment options unavailable at standard nail establishments. These facilities employ Certified Master Pedicurists who use sterilized instruments and dry techniques specifically designed to treat toenail fungus without causing further spread. Unlike conventional nail salons, these specialized centers offer private, one-on-one sessions lasting 45-60 minutes that include thorough assessment, cleaning, sanding, and application of antifungal products.
Medical-grade solutions like KeryFlex help remodel damaged nails while preventing fungal proliferation. For effective management of fungal conditions, these facilities recommend scheduling treatments every 4-6 weeks, particularly for high-risk patients. Athletes prone to nail fungus from excessive sweating and diabetic individuals benefit greatly from these specialized services that prioritize both treatment and prevention.
Medical Pedicures: A Professional Option

Medical pedicures represent a significant advancement in specialized foot care, offering thorough treatment options for individuals with nail fungus or other podiatric concerns. Performed by Certified Master Pedicurists in private settings with high hygiene standards, these treatments last 45-60 minutes and utilize sterilized instruments to safely address various foot conditions. Unlike traditional salon services, medical pedicures are dry procedures specifically designed to treat toenail fungus, corns, calluses, and ingrown nails through professional assessment and targeted interventions.
These specialized services provide three primary options: standard Medical Pedicure with dermabrasion, Antifungal Treatment using medical-grade products for infected nails, and Restore Treatment featuring KeryFlex for damaged nail remodeling. For best results, experts recommend scheduling sessions every 4-6 weeks, ensuring continuous care while maintaining the sterility necessary for treating compromised nails.
Post-Pedicure Care to Prevent Worsening Infections

Maintaining proper foot care after receiving a pedicure becomes essential when managing nail fungus, as neglecting post-treatment practices can greatly worsen existing infections or invite new ones. Daily cleansing with soap and water, particularly between toes, removes potential contaminants that could exacerbate fungal conditions. Thorough drying afterward is equally vital, as moisture creates an ideal environment for fungal proliferation.
To prevent the spread of infection, patients should trim nails straight across with sanitized tools, avoiding curved cuts that may lead to ingrown nails. Selecting breathable footwear and moisture-wicking socks effectively reduces dampness that promotes fungal growth. Daily monitoring for infection indicators—redness, swelling, or discharge—allows for prompt medical intervention, which research shows prevents complications in approximately 90% of cases when addressed early.
When to Postpone Your Pedicure Appointment

Knowing when to delay a pedicure appointment becomes essential for individuals managing nail fungus, as certain conditions may greatly increase infection risks or complicate existing problems. Clients should postpone appointments when experiencing throbbing pain, swelling, or redness indicating active infections that could spread during treatment.
Open wounds or cuts represent significant hazards, as the tools used during pedicures can introduce bacteria from contaminated water or equipment. Individuals with ingrown toenails or pincer nails should delay appointments, as standard pedicure techniques may exacerbate these conditions rather than improve them. Research confirms that improper handling of these conditions with typical salon tools can worsen outcomes.
Those with compromised circulation or diabetes face elevated risks during pedicures and should postpone until their foot health stabilizes, preventing potentially serious complications from routine salon procedures.
Treatment Options to Consider Before Your Next Salon Visit

Before heading to the salon with nail fungus, individuals should explore several treatment options that can improve their condition and guarantee a safer pedicure experience. Consulting a podiatrist for prescription antifungal medications is recommended, as these treatments target infections at their source, requiring 3-6 months for complete clearance.
Over-the-counter topical treatments containing terbinafine or clotrimazole, applied daily for 4-12 weeks, can reduce fungal growth before visiting nail salons. Medical pedicures, performed by Certified Master Pedicurists using sterile instruments, offer a controlled environment for treating toenail fungus. For persistent cases, specialized antifungal treatments with medical-grade products effectively penetrate the nail bed. Additionally, the KeryFlex Restore Treatment provides a resin-based solution that remodels damaged nails in one session, serving as both protective and cosmetic preparation for a standard pedicure with toenail fungus.
Frequently Asked Questions
Can You Still Get a Pedicure With Toenail Fungus?
Toenail fungus impact doesn’t completely eliminate pedicure options. Clients can still receive services if they inform salons beforehand, allowing for specialized precautions like sterilized tools and disposable items to prevent contamination risks.
Can I Get My Nails Done if I Have a Nail Fungus?
A study of 300 salons revealed varied policies on fungal infections. Clients with nail fungus can get manicures, but should inform technicians beforehand. Nail art options and color selection may be limited to accommodate proper infection control.
What Fungal Infection Would Prevent a Pedicure?
Severe onychomycosis, active tinea pedis, and fungal infections with secondary complications like cellulitis are fungal strains that prevent pedicures. Proper infection diagnosis by a healthcare provider is essential before seeking nail services.
What Should You Avoid if You Have Nail Fungus?
Individuals with nail fungus should avoid moist environments and shared footwear, as well as foot bath immersion, cutting toenails too short, rough tools, cuticle trimming, and using communal nail polish that may harbor contaminants.

